Notice of Admission – Payor Setup
Beginning January 1, 2022, Medicare will no longer require RAP submissions. Instead, for each admission, home health agencies will be required to submit a one-time Notice of Admission (NOA) within 5 calendar days of admission to the agency. Agencies will then only bill one invoice every 30 days. Sandata Agency Management has been updated to allow users to easily adopt these changes.
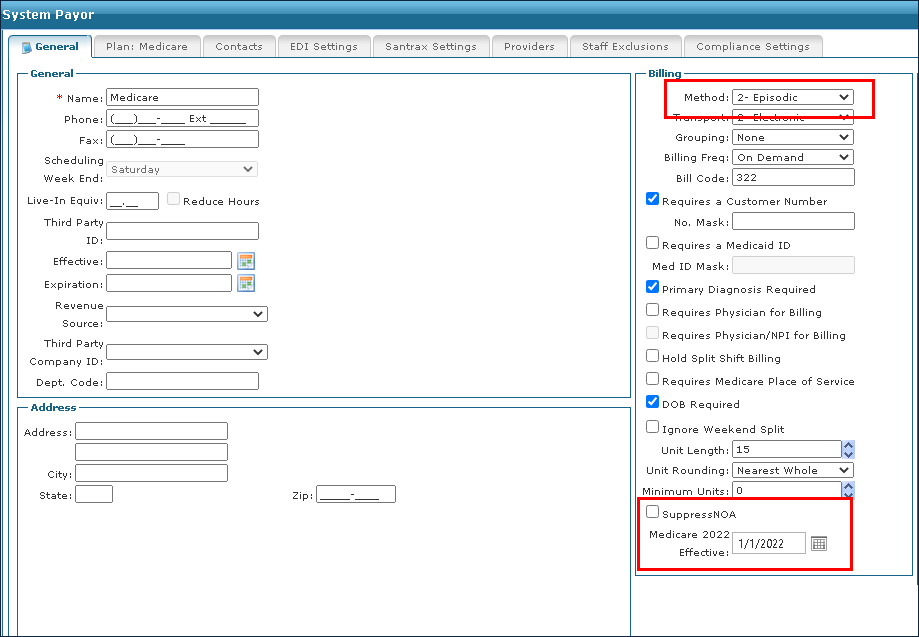
Updating the Payor file
| 1. | Locate the payor to be updated. |
Billing > Payors > Payor
| 2. | Confirm that the Billing Method is set to Episodic. |
| 3. | Enter the Medicare 2022 Effective Date. |
If the payor does not require an NOA, select the SuppressNOA check box.
| Note: If the Payor requires PDGM episodic billing and DOES NOT require RAPs and DOES NOT require a NOA, users will need to check the SuppressNOA checkbox and set the Medicare 2022 Effective Date. If no date is entered, the RAP rules would continue as they were in 2021. |

Comments
0 comments
Please sign in to leave a comment.