Creating a Notice of Admission for a New Client
Beginning January 1, 2022, Medicare will no longer require RAP submissions. Instead, for each admission home health, agencies will be required to submit a one-time Notice of Admission (NOA) within 5 calendar days of admission to the agency. Agencies will then only bill one invoice every 30 days. Sandata Agency Management has been updated to allow users to easily adopt these changes.
| Note: Before completing the process to create and submit an NOA, make sure you have set up your Payor correctly. |
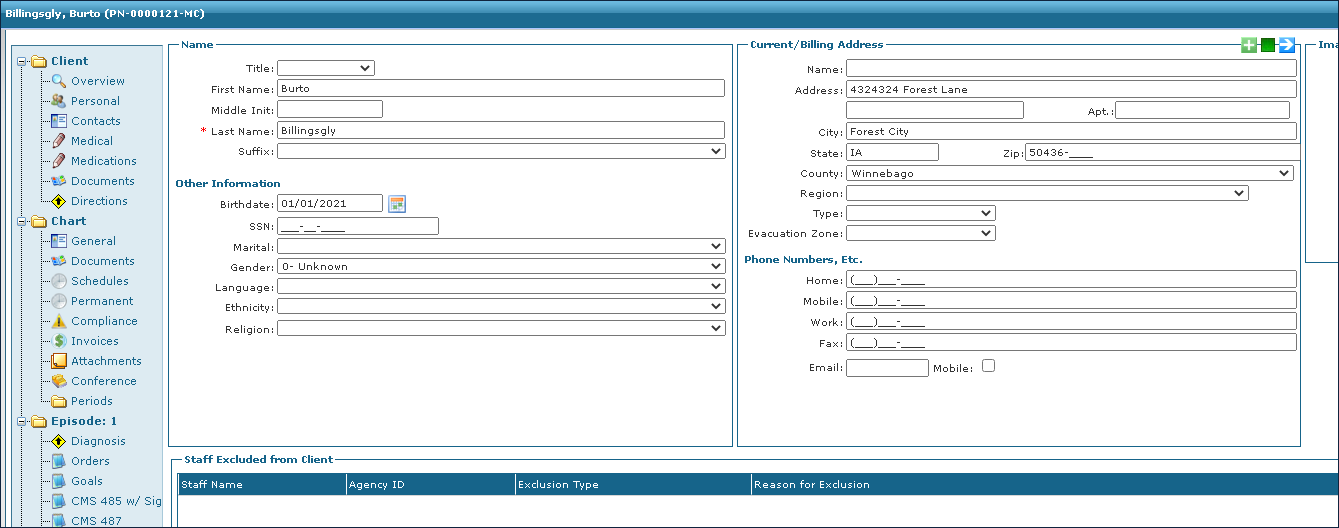
| 1. | Create the new client as normal. |
Ensure the following fields contain information to populate the NOA.
| A. | Client First and Last Name. |
Ensure this matches the client’s Medicare ID card.
| B. | Client Address |
| C. | Client Birthdate |
| D. | Client Medicare Beneficiary Identifier (MBI) |
| E. | Principal Diagnosis Code. |
This can be any valid diagnosis code.
Once the first billable visit has been completed:
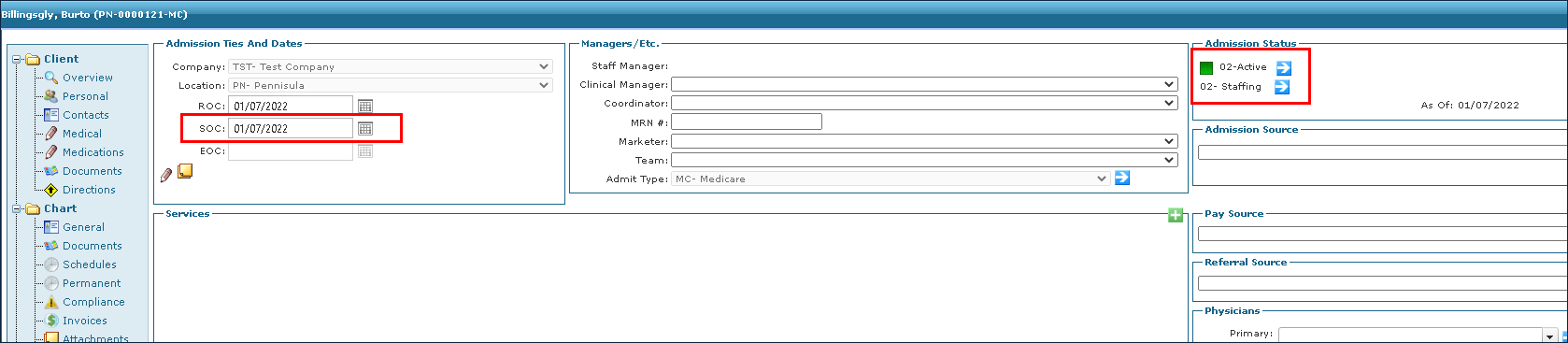
| 2. | Navigate to the General tab on the client’s chart. |
Client > Client Name > General
| 3. | Change the Admission Status to Active. |
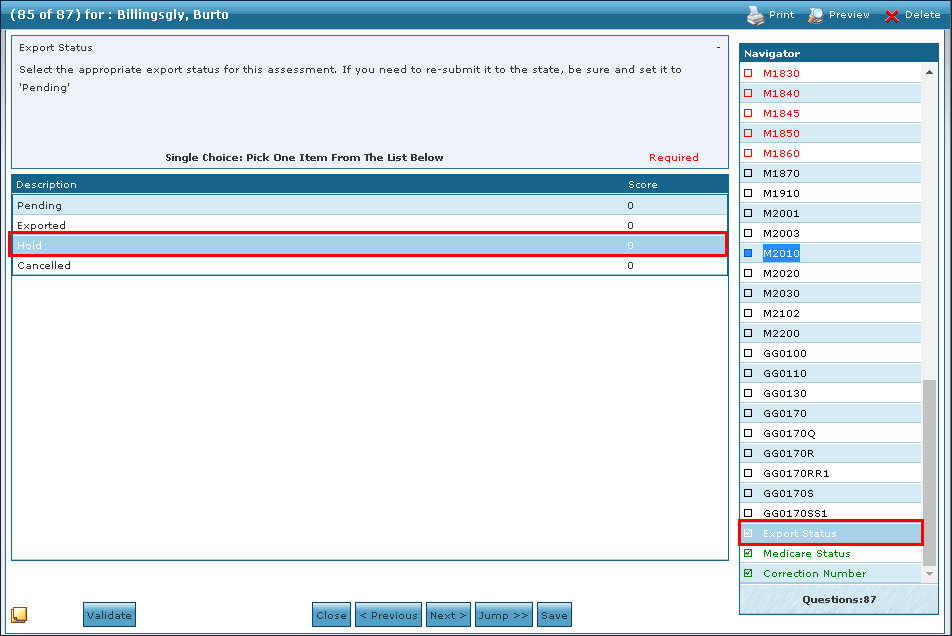
| 4. | Create a Start of Care (SOC) OASIS for the client. |
This can be either a full or Skinny OASIS.
| 5. | Change the Export Status to Hold. |
For a completed OASIS, the status can be changed to Pending. This prevents the OASIS from being sent and creates a NOA in RAP Ready status.
| 6. | Re-open the OASIS. |
| 7. | Review the data in the OASIS by clicking Next. |
| 8. | Click Finish. |
This creates the Final claim with a status of Pending or RAP Paid.
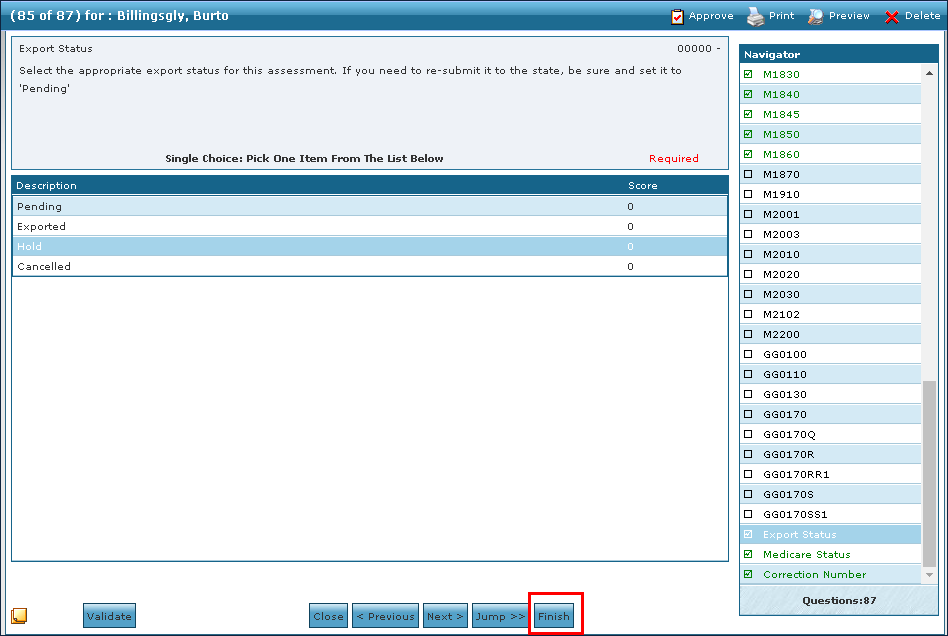
There are now two invoices in the Episode Tracker for the first period only. One for the Notice of Admission and one for the Final claim for the 30-day episode.
If the claim is in RAP Paid status, the claim is ready to be billed at the end of the 30-day episode.
If the claim is in Pending status, there is something missing from the claim. Double check that all necessary information has been entered, verify that any visits for the claim have been added and confirmed or verify that the OASIS has been completed. Once corrected, the claim automatically updates to RAP Paid status.

Comments
0 comments
Please sign in to leave a comment.